Arthritis and arthritis are diseases characterized by pathological changes in the joints, but the difference between arthritis and arthrosis is significant. To understand the difference between arthritis and arthrosis, it is necessary to consider the etiological factors, pathogenesis, symptoms of arthritis and arthrosis. The treatment of arthrosis and arthritis also has different approaches.
What is arthritis, arthrosis? How are joint lesions manifested in arthritis and arthrosis, what is the difference? In arthrosis and arthritis, the differences are a consequence of the mechanism of pathological changes.
Treatment of arthrosis and arthritis is long-term, multi-component. Often, as a result of untimely treatment, arthritis and arthrosis can be considered consecutive stages of the pathological process. Having understood what arthritis and arthrosis are, we will determine the differences between arthrosis and arthritis.
Arthritis, classification
Arthritis - due to inflammatory changes, it combines the pathology of the joints themselves, and is a symptom of other diseases that occur due to their defeat. How to treat arthritis depends on determining the cause that caused the inflammatory process.
According to the etiological factor, they differ:
- Primary - rheumatoid, rheumatoid arthritis, ankylosing spondylitis, Still's disease, etc.
- Secondary - complications of an infectious, non-infectious process (reactive to chlamydial infection, hepatitis, diseases of the gastrointestinal tract, septic lesions).
By the number of affected joints:
- Monoarthritis - with the defeat of one joint.
- Polyarthritis - when a group of joints is affected.
According to the nature of the course of the disease:
- Acute arthritis - with a vivid clinical picture of inflammatory changes in the connective tissue of the joint.
- Subacute - medium option, the phase of resolving the acute condition.
- Chronic arthritis - with an erased clinical picture, a slow course, periods of weakening and exacerbation.
Osteoarthritis, classification
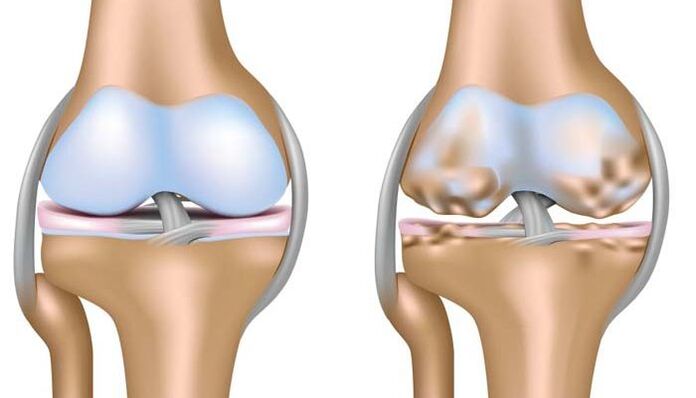
Deforming osteoarthritis, rheumatoid arthritis or arthrosis is a disease based on degenerative changes associated with the destruction of all joint structures, cartilage, ligaments, muscles, tendons and bones. This is the main difference between arthrosis of the joints and arthritis, which leads to irreversible deformities of the affected joint surfaces, dysfunction and disability of the patient.
- Idiopathic - no known cause. The pathological process is based on an autoimmune damage mechanism (primary rheumatoid arthritis in young patients).
- Secondary osteoarthritis is the result of metabolic disorders, trauma and inflammation. For example, rheumatoid arthritis that developed after you got over rheumatoid arthritis.
Arthritis, causes
Risk factors are:
- Violation of metabolic processes in the body.
- Hereditary predisposition factor.
- Infectious diseases.
- Conditions of immunodeficiency, presence of autoimmune diseases, allergic manifestations.
- Increased load on the musculoskeletal system due to professional activity, traumatic component.
Arthrosis, causes
Risk factors for the development of osteoarthritis are:
- Age. Osteoarthritis is a disease of the elderly, with the exception of rheumatoid arthritis, which occurs in adolescence. According to WHO statistics, about 10% of the world's population suffers from arthropathies.
- Physical overload, injuries, excess weight, which increases the load on the joint. Large joints suffer more than others: hip - coxarthrosis, knees - gonarthrosis.
- Hereditary factor: characteristics of metabolic processes, cartilage tissue structure.
- Previous inflammatory processes without appropriate therapy.
Arthritis, symptoms

Regardless of the cause of the disease, the signs of the disease have a similar clinical picture in the acute phase of the process and in the period of worsening of the chronic course of the disease.
- Pain is the first symptom. It has different intensity, is more often permanent, does not depend on physical activity.
- Hyperemia of the skin of the joint area, local increase in temperature (the joint area becomes hot to the touch), pronounced edema.
- The presence of effusion (fluid) in the cavity of the joint bag. Microbiological and cytological examination of fluid from an inflamed cavity is important for establishing a diagnosis and determining the causative agent. The knee joints are more often affected. The presence of the inflammatory nature of the fluid inside the joint capsule is the difference between arthritis and arthrosis of the knee joint.
- Extraarticular manifestations of the underlying disease: fever, vascular damage - vasculitis, heart valves, lung diseases - alveolitis, pneumonia, kidney damage - nephritis, skin manifestations, hematological changes - anemia, increase in the number of platelets in the peripheral blood.
- Limitation of range of motion in the joint, dysfunction.
Osteoarthritis, symptoms

Symptoms of arthrosis are caused by long-term malnutrition, blood supply to the cartilage plate. Cartilage loses its elasticity, becomes thinner, and outgrowths form from the bone tissue inside the joint cavity - osteophytes, which irreversibly deform the joint surface, impair functionality, cause pain and significantly limit mobility.
- Pain. The onset of the disease is characterized by moderate intensity, painful, constant pain. The strengthening of the pain syndrome is associated with an increase in dystrophic changes in the cartilage and deformities. Pain can vary, be temporary: from morning stiffness, to constant and disappear during the day. A rapid, intense increase in pain is a poor prognostic sign.
- visible deformation.
- Functional disorders: flexion, extension.
- Characteristic crunching when moving.
- The development of joint immobility leads to the disability of patients.
Osteochondrosis is a common pathological condition of the spine, which is based on the same changes in cartilage as in arthrosis.
Diagnostics

The diagnosis of arthritis and arthrosis aims to identify the root cause of the disease, determine the degree of activity of the process, assess the prognosis and effectiveness of treatment, and timely diagnose complications of the disease.
The complex of diagnostic tests includes general clinical laboratory tests, instrumental studies of the liver, kidneys, X-ray diagnostic measures, microscopic, bacteriological studies.
- Special characteristics of arthritis of different etiologies are: increase in erythrocyte sedimentation rate, increase in the level of leukocytes in peripheral blood, which makes it possible to determine the severity of inflammatory changes, increase in C-reactive protein in blood plasma. - an important laboratory diagnostic test.
- X-ray examination allows you to see a characteristic picture of inflamed joint surfaces.
- MRI is the most informative method for detecting inflammatory changes within the joint capsule.
- Doppler ultrasound is used.
- In severe cases, it is possible to perform arthroscopy for the purpose of differential diagnosis and treatment.
A fairly informative method that allows you to make a diagnosis, distinguish between arthrosis and arthritis is an X-ray examination. Depending on the identified changes, the degree of deformation of the intra-articular cartilage and the width of the joint space, there are four degrees of pathological changes in arthrosis.
Arthritis, treatment principles

Arthritis treatment is long-term, the main goal is to cure the disease that caused inflammatory changes in the joint capsule or achieve a long-term course of the disease without recurrence, prevent the development of irreversible changes, deformities, improve the quality and life expectancy of patients.
Widely used for treatment:
- Medical methods of influence. Depending on the etiological factor, the following are used: antibacterial, non-steroidal anti-inflammatory drugs, hormones, introduction of anti-inflammatory drugs directly into the joint cavity, chemotherapy drugs are prescribed for more severe forms of rheumatic disease.
- Treatment without drugs. An important role is played by physiotherapy exercises, adherence to diet, healthy lifestyle - quitting smoking, alcohol, physiotherapy, timely orthopedic care and correction of existing disorders, prevention of worsening of concomitant diseases.
- The surgical method is not the method of choice in treatment. This is a means to help patients in particularly difficult cases - with the development of severe complications, severe pain syndrome, ineffectiveness of the first two treatment methods. It has limitations and certain indications for appointment.
Osteoarthritis, treatment

Rheumatoid arthrosis is treated in a complex, including:
- Therapy without drugs. In rheumatoid arthritis, treatment includes physical therapy exercises, physiotherapy, protective regimen, load reduction, diet, weight loss.
- Medical treatment is associated with pain relief. Non-steroidal anti-inflammatory drugs, hormonal drugs are prescribed more often.
- Surgical treatment methods: plastic, arthrodesis, prosthetics of large joints (knee, hip).
Prevention of exacerbations
Due to the possibility of a long-term, chronic course of the disease, the development of complications, regardless of the cause of their occurrence, patients are subject to constant or long-term observation, rehabilitation measures designed taking into account individual characteristics and the nature of the disease. disease.
Important preventive values are:
- Treatment of inflammatory diseases of the musculoskeletal system, a complex of rehabilitation measures after injuries.
- Load limitation, healthy lifestyle, proper rational nutrition as a factor in the fight against excess weight.
- Timely orthopedic correction of bone deformities acquired during life.
Remember, at the first signs of problems, it is important to contact a specialist in a timely manner. Late initiation of treatment increases the risk of possible negative consequences of the disease.



















